ACOs incentivize better care quality for CMS patients – Centers for Medicare and Medicaid Services. Hospitals, providers, and other healthcare partners form the organization, coming together to coordinate high-quality healthcare for the sake of lowering costs among the patient population. Performance outcomes that are above the benchmark result in shared savings, which can be dispersed to member physicians. Precise and detailed reporting is imperative to achieving the highest score.
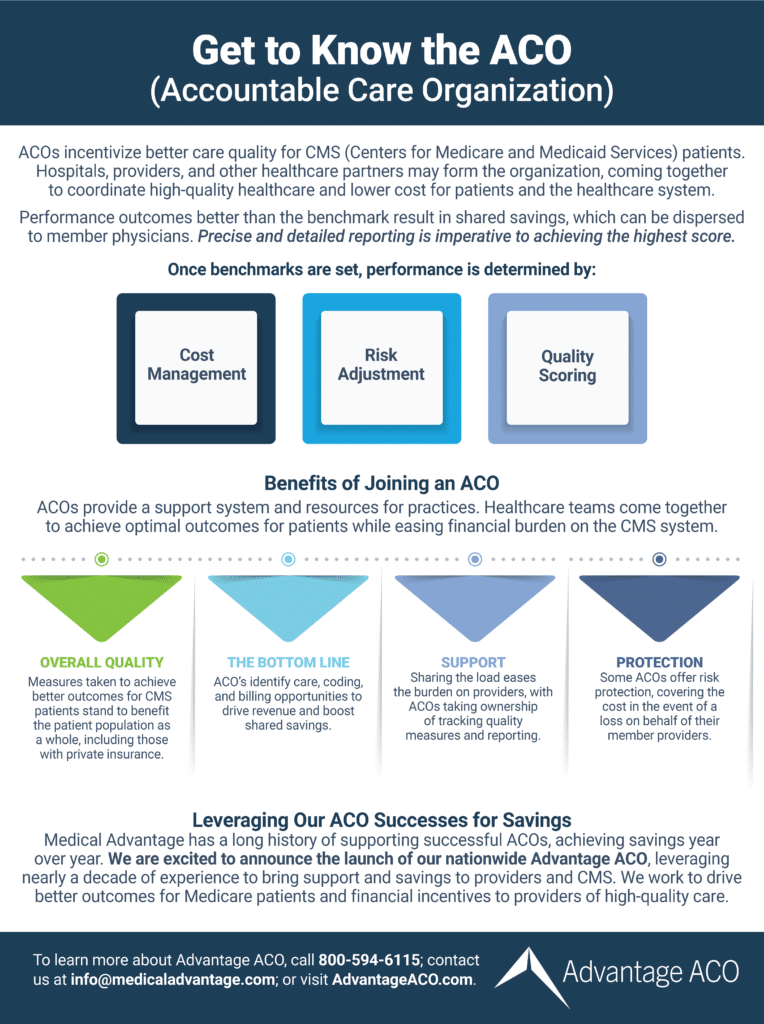
Once benchmarks are set, performance is determined by:
- Cost of care among the patient population.
- Cost of risk adjusted accounting for high-risk patients.
- Quality scoring.
Benefits of Joining an ACO
ACOs provide a support system and helpful resources for practices. Healthcare teams come together to achieve optimal outcomes for patients while easing financial burden on the CMS system.
- Overall quality: Measures taken to achieve better outcomes for CMS patients stand to benefit the patient population as a whole, including those on private insurance.
- The bottom line: ACO’s identify care, coding, and billing opportunities to drive revenue and boost shared savings.
- Support: Sharing the load eases the burden on providers, with ACOs taking ownership of tracking quality measures and reporting.
- Protection: Some ACOs offer risk protection, covering the cost in the event of a loss on behalf of their member providers.
Leveraging our ACO Successes for Savings
Advantage ACO has a long history of supporting successful ACOs, achieving savings year over year. We are excited to announce the launch of our nationwide Advantage ACO, leveraging nearly a decade of experience to bring support and savings to providers and CMS. We work to drive better outcomes for Medicare patients and financial incentives to providers of high-quality care.

